The information on this website should not be considered medical advice.
This website contains affiliate links, and we may be compensated for referrals.
How To Write a Prescription (With Examples)
What are prescription medications?
In the United States, the dispensation of certain drugs is regulated by the Food and Drug Administration (FDA). These drugs are known as prescription medications because they can only be obtained by consulting a prescriber first. Prescription medications are classified as Rx-only.
Some prescription medications have a potential for misuse. These medications are classified as Schedule I – Schedule V. Schedule I medications, such as heroin, are illicit drugs considered to have no therapeutic value. They cannot be prescribed. Schedule II drugs are considered to have a high risk of misuse; these drugs are closely monitored but have therapeutic value that outweighs the risk in some cases. Examples of schedule II drugs are Adderall and oxycodone. Rx-only drugs that don’t fall under Schedule I – Schedule V have not been identified as carrying a risk of misuse. Note that a drug’s schedule only categorizes its potential for misuse and does not represent all aspects of its safety profile. Some drugs are available without a prescription, over the counter or, “OTC”.

Who is a prescriber?
What is an Rx number?
Why is it important to regulate how every prescription is written?
While we may not realize it, medication errors are still a big issue that the healthcare industry faces. The only way to combat errors is to make sure every prescription is written in the same format.
Medication errors are very costly both monetarily and in patient morbidity and mortality. The statistics are alarming, and medication errors remain a major reason why malpractice insurance is incredibly high for healthcare practitioners. Learning early on how to check and recheck prescriptions can decrease a lot of stress for both patients and practitioners. Every detail of the prescription matters. For example, writing the patients identifying information prior to signing the prescription is important if using a written pad, as losing a signed prescription with no name can be dangerous if it falls into the wrong hands.
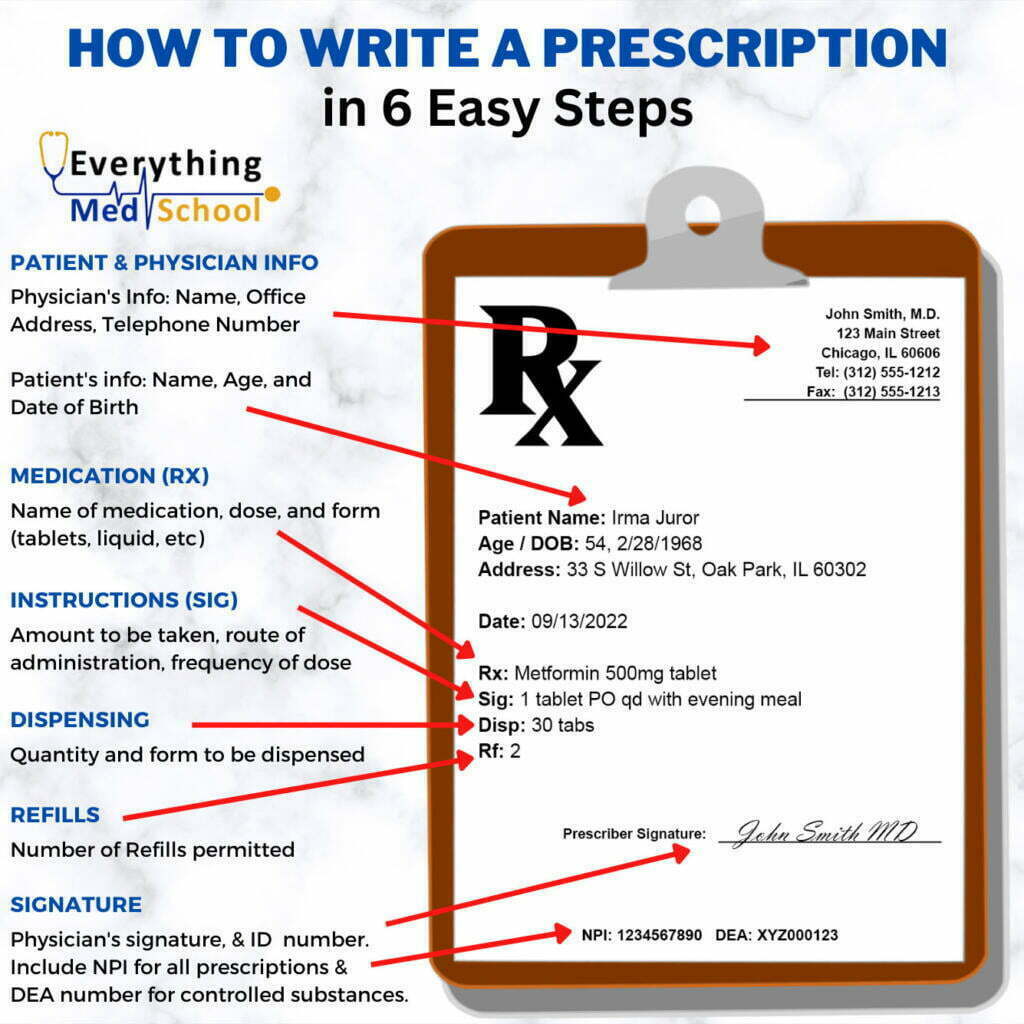
How to write a prescription
A prescription MUST include the following:
- Patient identifying information: This includes the patient’s full name, date of birth, and (usually) home address. This generally is in the middle of the bottle below the practitioner’s information.
- Practitioner’s identifying information: This includes the practitioner’s full name, NPI number, and signature. It often includes the clinic address as well as the office phone number if the pharmacist needs to contact the prescriber with any questions.
- They will also need to add a DEA number if prescribing controlled substances such as opioids, ADHD medication, anti-anxiety medications, certain sleep aids, and more.
- Recipe (Rx): This includes the name of the medication, the dosage, and the dose form. For example, if the clinician is prescribing 800-milligram tablets of Ibuprofen, it would be written as Ibuprofen 800 mg tablets or tabs.
- Also, medications come in many strengths, so if the pharmacy is not carrying 800 mg tablets, they can adjust with their 200 mg tablets and still dispense the correct amount to the patient.
- It is also important to specify if the brand name medication is the only option or if a generic medication can also be prescribed!
- Instructions, also known as the signature, using sig codes (see below for the most common sig codes used by physicians):: Amount to be taken, route of administration, and frequency of the dose
- For example, continuing with the Ibuprofen example from above, if the clinician is prescribing one tablet of 800 mg of Ibuprofen every 8 hours, they would have to write “take one tablet by mouth every 8 hours” or if they use the sig codes they would write “1 tab po q8”.
- A clinician can also prescribe medications as needed, which can also be labeled as PRN. So if they are prescribing Ibuprofen for pain as needed, they must specify “1 tablet by mouth every 8 hours as needed for pain” or “1 tab po q8 PRN”. If a medication is PRN, why the medication is to be taken must be specified. For example, “PRN for anxiety” or “PRN for headache.”
- Dispensing instructions: This is imperative to let the pharmacist know how many tablets to include in the prescription. Writing the quantity clearly is very important so as to not over- or under-dispense to the patient. With our Ibuprofen example, if the clinician would like to provide a 30-day supply, it’s important to write the number of tablets (which would be 90 tablets if the pill were to be taken 3 times a day, or every 8 hours).
- Refill Instructions: This will come after the dispensing instructions, and it’s imperative to include exactly how many times the patient can refill this medication. Even if it is a one-time prescription, the clinician must write zero refills.
- Date: Including the date of the prescription is important to make sure patients do not attempt to refill their medications earlier than they are prescribed for.
In this example, the patient, Irma Juror, will be able to use their date of birth and address to verify their identity with the pharmacy. They have been prescribed Metformin in 500mg tablets. The patient has been instructed to take 1 tablet by mouth every day with their evening meal. Prescriptions are typically written in 1-month or 3-month supplies. In this case, the patient is given a 1-month supply of 30 tablets and two refills, so they will have enough medication for three months before they need to visit their prescriber again. The quantity is sometimes written with a # sign before it to differentiate it from other numbers on the prescription, such as the strength. They may also be able to request refills electronically or over the phone, either through their doctor’s office or through the pharmacist, who will contact the doctor’s office for them.
While this can feel very daunting as a medical student and new resident physician, after a bit of practice and consistently following the steps above, it will feel easy and natural. Especially with the predominant way to prescribe being via the computer, there are systems in place to double-check prescriptions and ensure there are no contraindications between the patient’s home medications and the new medications being prescribed.
To get more information on the signature (sig) codes that practitioners use to abbreviate their prescriptions, read below!
Prescription abbreviations and sig code meanings
| ad | right ear |
| APAP | acetaminophen or Tylenol - short for N-acetyl-p-amino-phenol |
| as | left ear |
| au | both ears |
| bid | twice a day |
| cap | capsule (cannot use interchangeably with tablet) |
| DAW | dispense as written - if written for a brand name medication, indicates that the generic version may not be substituted |
| DEA | drug enforcement agency - some prescribers have a DEA identification number that allows them to prescribe controlled substances |
| gtt | drop |
| NPI | National Provider Identifier - a unique 10-digit identification number for healthcare workers |
| od | right eye |
| os | left eye |
| ou | both eyes |
| po | by mouth |
| prn | as needed |
| q4h | every 4 hours |
| q6h | every 6 hours |
| qd | every day |
| qhs | every night at bedtime |
| qid | 4 times a day |
| qod | every other day |
| sc | subcutaneously |
| sig | directions |
| tab | tablet (cannot use interchangeably with capsule) |
| tid | three times a day |
Prescription Examples
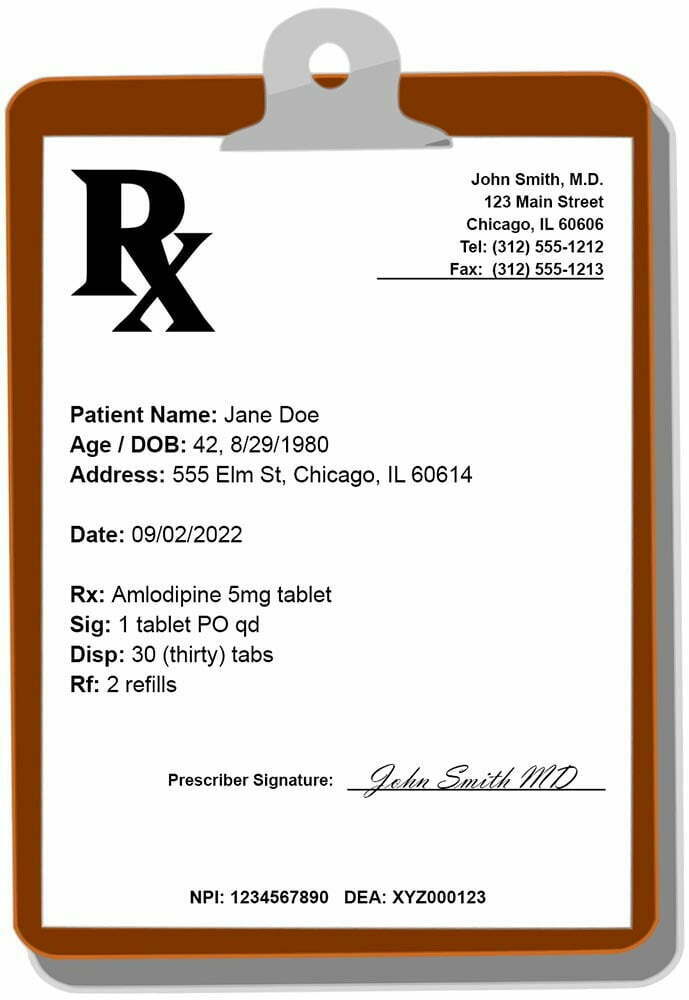
Example of a regular prescription
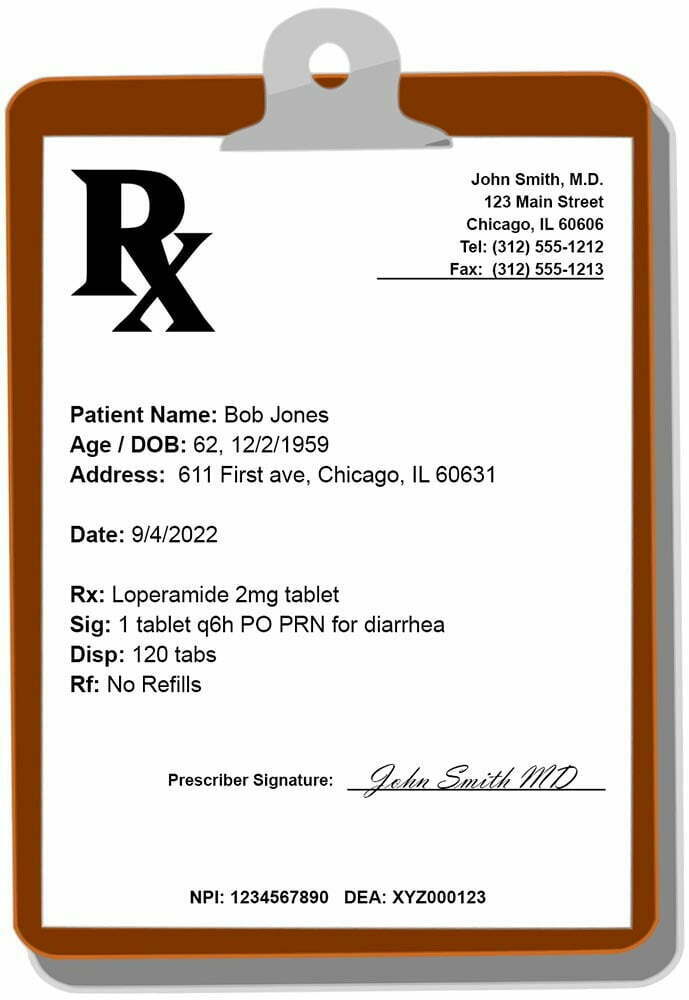
Example For PRN and to calculate out tablets for dispensing
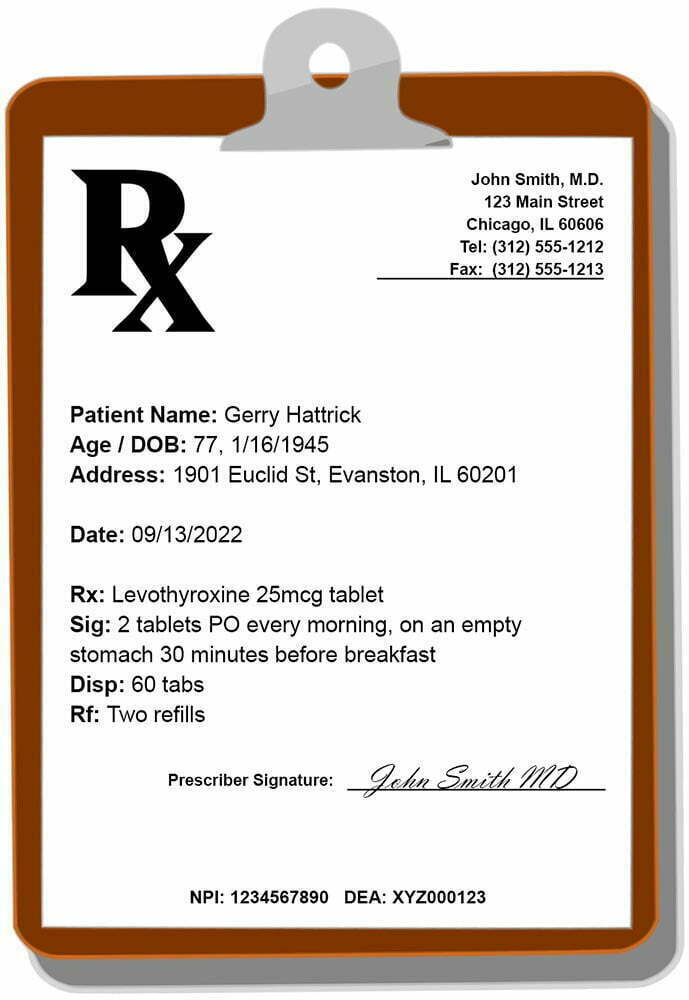
For specific dosing/timing & to calculate tablets for dispensing
Facebook Comments
Ankita Kadarmandalgi graduaged from Touro College of Osteopathic Medicine and is an anesthesiology resident at Rush University Medical Center. Her interests include weight training, listening to podcasts, and hanging out with friends.